 The New Science of Hair Growth Download PDF
The New Science of Hair Growth Download PDF
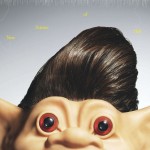
Robot follicular surgeons, invisible micrografts, in vitro hair cloning … scientists have a wider array of weapons than ever before in the war on baldness. Many believe we’re finally on the verge of banishing it forever.
Brandishing a syringe the size of a caulking gun, hair-transplant surgeon James Harris, MD, injects local anesthetic into the scalp of a male patient, a married financial analyst in his early forties who has asked not to be identified. We’ll call him Scott. For five hours, I’ve been watching Dr. Harris perform a hair transplant called surgically advanced follicular extraction, or SAFE. A follicular unit is a miniature, self-contained hair factory embedded in the skin. Each square centimeter of human scalp contains 80 to 120 follicular units, and each of those has one to four hairs.
Though Scott is sitting upright, his scalp is a gruesome battlefield. Rivulets of blood seep from thousands of BB-size puncture wounds. A trash can is brimming with blood-soaked gauze. But Scott feels nothing. He’s watching CNBC’s financial roundup on a wall-mounted TV while thumbing through e-mails on his BlackBerry, oblivious to the mayhem topside.
Dr. Harris is using a motorized tool he designed himself, in a procedure that, for all its bloodshed, represents the current state-of-the-art in baldness treatment. The instrument has a blunt hollow tube that lets Dr. Harris make incisions less than a millimeter wide, in rapid-fire succession, around clusters of hairs without damaging the underlying follicles. It’s painstaking work. I watched earlier as Dr. Harris donned mantislike headgear (dual loupes with six-fold magnification) and extracted follicular units from a band of hair between Scott’s ears, a region of scalp hair docs call the “horseshoe fringe.” In virtually all men, this fringe is impervious to balding, a vestigial result of genes that dictate how skin forms during fetal development.
By the time he’s through, Dr. Harris will have made 1,045 incisions along the front and top of Scott’s head, enough to accommodate the same number of follicular units removed from his fringe. An assistant counts the extracted follicular units under a microscope, tabulating the number of individual units and the number of hairs protruding from each one. Single hair units are reserved for the front to create a feathered widow’s peak. “I want to avoid a wall of hair jutting from the forehead,” explains Dr. Harris, citing a common blunder of botched transplants. “SAFE is a lot less traumatic than other transplant procedures, such as a surgery in which a strip of scalp is extracted, because it’s minimally invasive.” Even so, the procedure looks medieval, and it’s hard to believe this gory mélange will have a happy ending.
Hair transplants have improved dramatically in the past 10 years, although in the hands of unskilled surgeons, mishaps can occur that leave patients with gruesome doll heads. But transplants remain hamstrung for a more fundamental reason: You can shuffle only so many hairs from fringe to forelock. This is Scott’s fourth surgery, and at this point he’s simply running out of hair. It’s a dwindling game of musical chairs that confounds surgeons and frustrates patients. The average age for undergoing a hair transplant is 40, but hair is doomed long before that. To be precise, its fate is decided in utero, during the tenth week of pregnancy, when the human fetus is the size of a peanut shell. That’s when the fingers and toes take shape and the brain starts to evolve. It’s also when the hair follicles form—roughly 5 million over the entire body. This number is fixed: After exiting the womb, the human body can’t produce a single additional follicle. That’s why a revolutionary technique known as hair cloning, or hair multiplication, holds so much promise. It changes the game because it gives transplant surgeons an endless supply of follicular units to restore the vanishing manes of their patients. Researchers in a handful of labs around the world have been testing the technique on mice with impressive results. Several start-ups have formed, and these companies are racing to complete successful human clinical trials. It could have a profound effect on the landscape: Male pattern baldness, or androgenetic alopecia, affects 40 million men in America. Although it doesn’t have any known physical downsides, the specter of premature aging and the perception of waning virility and diminished sexual attractiveness can be mentally debilitating and lead to personal, social, and work-related problems, according to Nigel Hunt, PhD, an Associate Professor of Applied Psychology at the University of Nottingham, in England. In 66 percent of men, hair follicles start to shrink around age 35 (in some men, it starts at age 21), causing hair to thin. By age 50, hair follicles are dying and 85 percent of men have significantly thinning hair. For these men, the cure for balding can’t come soon enough.
THE DAWN OF HAIR CLONING
The eureka moment for Colin Jahoda, MD, PhD, and Amanda Reynolds, PhD—a husband-and-wife team of biologists at the University of Durham, in England—involved an experiment that also served as a nerdy version of a “Colin Forever” tattoo. Dr. Jahoda removed a hair follicle from his head, put it under a microscope, and snipped off a cluster of dermal papilla cells, which are located in a bulb at the root of the shaft. He then nicked his wife’s forearm with a scalpel and transplanted the cells. A few days later, a thick tuft of dark hair (complete with Dr. Jahoda’s male DNA) emerged. The experiment demonstrated, for the first time, the possibility of growing hair from transplanted dermal papilla cells. It seemed the two had found a new treatment for hair loss. Yet they soon discovered that, once removed from the body, dermal papilla cells quickly lose their ability to make hair if they are not transplanted immediately.
Angela Christiano, PhD, a professor of dermatology and genetics and development at the Columbia University College of Physicians and Surgeons, collaborates closely with Dr. Jahoda on hair-related research. “Not long after you remove them, the cells don’t even know they’re dermal papillae anymore,” says Christiano, who is sitting in her office behind a desk piled two feet high with books and papers. “It’s like taking an Etch-a-Sketch and shaking it,” she says. “You erase their identity.”
The Jahoda-Reynolds experiment worked because a clump of hair follicle cells were promptly relocated, which preserved their inductivity, a measure of their capacity to remain uniquely hair cells before devolving into something more generic. While I’m in her office, Christiano calls England and puts Dr. Jahoda on speakerphone. “These cells seem to have an in-built regulatory system,” he explains. “We don’t know how it works. Getting the cells to remain inductive is still the basic challenge.”
Christiano became interested in hair follicle research in 1996, when a common hair disorder called alopecia areata caused patches of her own hair to fall out abruptly (steroid injections have revived it to a formidable whorl of ebony locks). Two years later, she made headlines after announcing she’d pinpointed several specific genes that are responsible for other genetic forms of hair loss—a scientific first. She is now focused almost exclusively on finding new genes for hair loss, as well as using dermal papilla cells to develop new ways of treating it. Scientists are still unclear about precisely what occurs, but they do know that whenever you pluck or shave a hair, molecular compounds in the follicle begin a complex dialogue with surrounding cells. These include dermal papillae, epithelial cells (those lining the wall of the hair shaft), and stem cells in a little understood region referred to as “the bulge.”
The dermal papillae are encoded with genetic instructions that respond to cues sent from surrounding cells and tissues in the follicle. Once signaled, the dermal papillae begin hatching hair fibers. What Christiano and Dr. Jahoda are trying to figure out is how to trick the cells into growing hair by themselves, without guidance from the rest of the follicle. Doing this would allow scientists to culture, or clone, thousands of dermal papilla cells in the lab that would retain their knack for producing hair. “With current transplant surgery, if you take a thousand follicles from the back of the head and move them to the front, you still only have a thousand,” says Christiano. “With the cloning approach, you could start with a small biopsy of cells and then grow enough of them to repopulate your entire scalp with hair.”
A researcher named Claire Higgins informs us she has just received a fresh dime-size chunk of live scalp donated by a male hair transplant patient. We join her in a lab, where she is hunched over a steel table, staring into a microscope. With forceps and a long needle, she scrapes dermal papillae from each follicle. I look through the eyepiece. She tells me I’m viewing roughly 3,000 dermal papillae packed into a ball of cells just a fraction of a millimeter wide. They resemble golden tobiko, the flying-fish roe dolloped onto sushi rolls. These cells will end up in an incubator, where they’ll be cultured for at least four weeks and then transplanted into mice to see if they’ll produce hair.
Several factors determine whether this happens. One is the growth medium, the soupy broth fed to the cells to help them thrive. Another is how quickly the cells multiply: As Dr. Jahoda and Reynolds showed, the less time cells spend outside the body, the better they retain their inductivity. A third factor is how the cells are transplanted. Do you inject them? Or position them surgically under the skin? “We’re trying to get into the heads of the dermal papillae and understand why they lose their inductivity,” says Christiano. “Then we’ll do the reverse: Take old cells that have been in culture for many months and bring them back into the fold, coaxing them to grow hair.”
I ask Christiano how she and Dr. Jahoda intend to accomplish this. She smiles, clearly not wanting to tip her hand, and replies, “We have a few ideas. I will say that if we figure it out, a lot of hair-loss sufferers will be very, very happy.” Their research could also inform next-generation baldness cures, genetic fixes that reprogram the cells, much like a software patch, and override the genes responsible for androgenetic alopecia.
TRAINING HAIR CELLS TO GROW
Nude mice are the foot soldiers for the war on balding. These dainty pink-hued rodents have been bred or genetically altered to remain hairless throughout their lives. They can be ordered by the mischief-load from medical suppliers and endure poking and prodding and other unspeakable horrors for the sake of balding men everywhere. In Philadelphia, Ken Washenik, MD, PhD, executive vice president of scientific and medical development for Aderans Research Institute and a clinical assistant professor of dermatology at New York University’s Langone Medical Center, shows me slides of nude mice on his laptop. They have undergone a new type of hair cloning procedure that Dr. Washenik has been developing for Aderans. The company, which has its headquarters in Tokyo, is the world’s largest manufacturer of wigs. It also owns Bosley, which operates 88 hair-transplant clinics in North America.
When I arrive at Aderans, Dr. Washenik hastily ushers me past several labs, perhaps wary I might glimpse some sort of trade secret, and into an empty conference room. What he does reveal is that his approach to hair cloning (he calls it follicular neogenesis) doesn’t rely solely on dermal papillae. “We are using a two cell construct, growing not just dermal papillae but also another type of cell from the follicle,” he explains. As the thinking goes, disparate cell types already communicate with one another in the follicle to regenerate hair. Dr. Washenik believes that if he can re-create that environment in the lab, cultured cells won’t get dementia and forget how to make hair. “The different cells in the follicle are smarter than we are,” says Dr. Washenik. “They already know they are supposed to be hairy. In eight days, we grew a ball of hair that never existed before on the back of a mouse.”
Dr. Washenik clicks an image file on his computer: The photo shows what looks like Piglet with a sable Mohawk. But there is a caveat: “These were hair cells from a mouse that were injected into a mouse. When researchers injected human cells into a mouse, they didn’t get the same results.” This disappointed Dr. Washenik and other researchers, because unlike other organs, follicles are supposed to be immune privileged: When transplanted across or between species, they’re expected to grow normally, without being rejected or provoking infection. He hopes to have better luck in clinical trials, when he will transplant human cells into humans. Aderans is in the second phase of a human trial, which is expected to be completed by the end of the year.
The company is pouring serious cash (Dr. Washenik won’t say how much) into its hair-cloning effort. Dr. Washenik is also intrigued by other researchers who are pursuing another pathway. They’re cultivating in vitro microscopic hairs, or “proto-hairs,” as Dr. Washenik dubs them. “These are early follicular structures that you can place in the scalp with the same technology that’s used for a hair transplant,” he says. “The big hurdle so far is getting the cells to multiply to make enough hair. Once we culture them, they sometimes die or de-differentiate.”
But Dr. Washenik remains confident. “The sooner we figure this out, the better,” he says. “So many people are waiting for this technology. I know that with every medical advance, the first one to market becomes the leader, and everyone else plays catch-up.” Like many of the scientists I meet, his passion for a cure is personal. “I started going bald at 25,” he says, tussling his hair to flaunt his 2,200-graft transplant. “While I was working on my PhD, I was mixing up homemade minoxidil [the active ingredient in Rogaine] in my lab.”
A few blocks away is a start-up called Follica. One of its co-founders, George Cotsarelis, MD, is a cutaneous biologist and associate professor of dermatology at the University of Pennsylvania. In 1990, Dr. Cotsarelis was investigating the biological mechanisms of skin regeneration. “I was studying stem cells and found a population of them in the hair follicle, in a strange area called ‘the bulge,’” he tells me when I stop by his office at U. Penn’s School of Medicine. “We didn’t know the function of the area, and we almost blew it off.” From then on Dr. Cotsarelis started paying more attention to hair follicles. After a series of more recent experiments on mice, he made two important discoveries. First, he found that bulge cells aid in the formation of new hair follicles, suggesting that these cells influence hair growth during embryonic development, when we were bobbing around in the womb. He also learned that, throughout our lives, these same stem cells awaken to mend minor cuts and burns, as well as deeper wounds in the skin. What baffled Dr. Cotsarelis is why, if a healing wound is populated with bulge stem cells, new follicles don’t form. The answer would at least explain why hair doesn’t grow from scars.
Dr. Cotsarelis conducted further studies designed to reveal what kinds of molecular compounds (e.g., hormones and proteins) are present during hair-follicle development in mice embryos and are also present in adult mice. A major one, which he wrote about in a 2007 Nature article, was something called Wnt (pronounced wint), a network of proteins first identified in fruit flies. Curious, Dr. Cotsarelis applied Wnt to small lesions purposely cut into nude mice (such gracious, noble critters). To his shock, follicles formed and sprouted hair. So if a person is bald, the obvious strategy would seem to be to douse his scalp with Wnt and wait for hair to grow. “The problem is that Wnt is involved in a lot of other things, one of which is skin cancer,” says Dr. Cotsarelis. “It’s very tricky business.”
The idea behind Follica is to develop a procedure in which a surgeon would lightly wound the scalp—something akin to microdermabrasion, an anti-aging treatment—to disrupt the skin and then apply a compound that would influence hair development in the area. This would trick the cells into reverting to an embryonic state, one in which they are genetically preprogrammed to make hair rather than simply repair skin, as they’re predisposed to do after we’re born. “Just when cells are deciding, ‘Do I make a hair follicle? Or do I make an epidermis?’ we can influence them with a protein to go down a hair-follicle pathway.”
TESTING THE SCIENCE ON HUMANS
My hair started thinning when I was 32. I’m now 40, and my hedding has eased up. Dr. Harris informs me I have plenty left for a follicular unit transplant. But after watching Scott’s procedure, I’m a little freaked out. Yet, all the specialists I speak with urge anyone dealing with hair loss to act fast, because once the hairs are gone, they’re gone for good.
“Absolutely no one concerned about hair loss should wait,” says Dr. Washenik. He started taking Propecia when he was in his thirties (he’s now 50), and he uses Rogaine religiously. He is a big advocate of drug therapies, and readily champions surgical options such as follicular unit grafting. Dr. Washenik examines my scalp and announces, “Rogaine is made for you. You’re not bald; your hairs are just miniaturized.” I’m a chemical-phobe, so I’d rather save my dough and wait for a viable hair cloning procedure, which many of the experts I talked to claim is less than five years away.
Intercytex, a public company based in London, may be closest to a marketable product, says Jerry Cooley, MD, a transplant surgeon who has been consulting for the firm since 2001. Nobody directly employed by Intercytex would speak to me for this story. “We do not feel that exposure of our research is helpful,” wrote Jeff Teumer, Intercytex’s director of research, in a curt e-mail. But Dr. Cooley, who works closely with Teumer, tells me that Intercytex scientists have successfully grown large batches of cloned proto-hairs similar to those that other researchers have been struggling to keep alive. What’s more, in animal experiments, the Intercytex team has observed cloned hair follicles growing hair again after the original hairs were plucked. This suggests that their cloned follicles cycle through the entire life span of hair—three phases known as anagen (growth), catagen (transitional), and telogen (resting)—something no other researchers have been able to do.
A key to the team’s success has been growing proto-hairs in a special medium, licensed from a Japanese inventor, which contains cultured skin cells known as keratinocytes. “I’m very excited about this technology,” says Dr. Cooley. “It’s not a matter of if, it’s a matter of when.”
Bessam Farjo, MD, a hair-restoration surgeon contracted by Intercytex to run its ongoing clinical trials, says, “All I can tell you is that we’ve grown a significant number of hairs on animals through this technique.” It sounds encouraging, and Dr. Farjo expects to complete clinical trials this year.
Hair cloning will be pricey initially, so early adopters may be men who are not only wealthy but also desperate because they don’t have enough hair left to do a follicular unit transplant. Cloning could also be ideal for younger men who aren’t good candidates for follicular grafting. “Younger guys aren’t suitable for current surgical techniques because we don’t know how much hair they are going to lose,” says Dr. Farjo. Imagine if the receded hairline of a 25-year-old male were replaced with a follicular unit transplant. If the rest of his hair were to fall out—and going bald at an early age generally means it will—he wouldn’t have enough hair to complete a second or third follicular unit transplant, so he’d end up with a solitary plume sprouting from his forehead. “It would look like unfinished business, which is why we typically avoid working on young guys,” says Dr. Farjo. “But if I know I’ll never run out of hair, thanks to the new cell therapy, I can treat anyone.”
Nobody is sure how the actual cloning process will be implemented. Most surgeons speculate that they’ll use boring tools similar to the existing ones used for harvesting follicular units. The follicular units will be sent to centralized labs, where industrial incubators will mass-produce millions of follicle cells for a relatively low cost. Another question is how will the cloned cells be transplanted? Instead of transplanting follicular units, your surgeon may inject cloned cells into micro-incisions, or he may implant lab-grown hair follicles. It could be fast, clean, and painless. Or it might entail something closer to Dr. Cotsarelis’s method at Follica. At Intercytex, technicians are tinkering with sundry techniques. “We’re experimenting with varying the number of cells in each injection, and whether we have to inject the cells into the skin as it is, or if we have to pre-stimulate the skin,” says Dr. Farjo.
Whatever the outcome, choices will abound. In the future, hair cloning will coexist alongside follicular unit transplants, drug therapies, and emerging technologies still incubating in the labs. For his part, Dr. Harris is also part of a team designing the world’s first follicular extraction robot: It will fully automate the procedure, making it magnitudes faster and less expensive. While Scott was being prepped for surgery, Dr. Harris took me into his office to show me a photo of the $25 million speed surgeon (the actual machine was locked in a storage closet a few floors above us). At about six feet tall with a fixed base and a mechanical arm with multiple joints, it resembles one of those space-age automatons you might see on a vehicle assembly line at a Toyota plant. Dr. Harris has already tested it on a couple of willing volunteers (with no alarming mishaps) and is preparing to apply for FDA approval under the name Restoration Robotics.
“We think the robot might be able to extract a thousand grafts an hour,” says Dr. Harris. “That’s more than triple what can be done by hand. This will broaden the market so that more people can afford the procedure. There may be a time soon when hair-transplant surgery will be available to everyone.”
Copyright © Michael Behar. All Rights Reserved.
